How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
What Causes Heel Pain?
 Heel pain can have a wide variety of causes, but the location of the pain can help to guide a proper diagnosis. Pain along the bottom of the foot can be caused by plantar fasciitis, heel pad syndrome, plantar warts, calcaneal stress fractures, nerve entrapment, or a neuroma. Pain in the middle of the foot can be due to peroneal tendinopathy, sinus tarsi syndrome, or tarsal tunnel syndrome. Pain in the back of the foot can be caused by Sever’s disease, Achilles tendinopathy, or a Haglund deformity. Seeing a podiatrist is the first step to healing your heel pain. A podiatrist will be able to examine your heel, ask questions about your current symptoms and medical history, and perform the tests necessary to diagnose and treat your heel pain.
Heel pain can have a wide variety of causes, but the location of the pain can help to guide a proper diagnosis. Pain along the bottom of the foot can be caused by plantar fasciitis, heel pad syndrome, plantar warts, calcaneal stress fractures, nerve entrapment, or a neuroma. Pain in the middle of the foot can be due to peroneal tendinopathy, sinus tarsi syndrome, or tarsal tunnel syndrome. Pain in the back of the foot can be caused by Sever’s disease, Achilles tendinopathy, or a Haglund deformity. Seeing a podiatrist is the first step to healing your heel pain. A podiatrist will be able to examine your heel, ask questions about your current symptoms and medical history, and perform the tests necessary to diagnose and treat your heel pain.
Many people suffer from bouts of heel pain. For more information, contact Dr. Thomas E. Silver of Westwood Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Can Sever’s Disease Affect Both Feet?
 Sever’s disease, also known as calcaneal apophysitis, is an overuse injury of the growth plate in the heel bone. This condition typically affects children between the ages of 8 and 14 who participate in sports or running and jumping activities. It is thought to be caused by the Achilles tendon pulling repetitively on the heel’s growth plate, creating tiny injuries that can become inflamed and painful. Sever's disease can affect either one foot or both feet at the same time. It affects both feet in about sixty percent of cases. This condition is typically treated with rest, footwear and activity modifications, and over the counter anti-inflammatory medications. If your child complains of heel pain, it is suggested that you take them to see a podiatrist right away.
Sever’s disease, also known as calcaneal apophysitis, is an overuse injury of the growth plate in the heel bone. This condition typically affects children between the ages of 8 and 14 who participate in sports or running and jumping activities. It is thought to be caused by the Achilles tendon pulling repetitively on the heel’s growth plate, creating tiny injuries that can become inflamed and painful. Sever's disease can affect either one foot or both feet at the same time. It affects both feet in about sixty percent of cases. This condition is typically treated with rest, footwear and activity modifications, and over the counter anti-inflammatory medications. If your child complains of heel pain, it is suggested that you take them to see a podiatrist right away.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
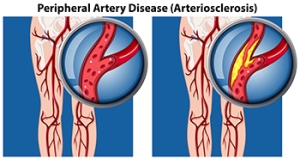
Signs of Peripheral Artery Disease
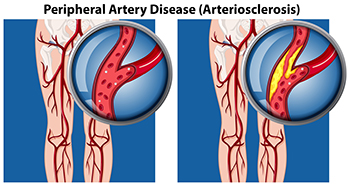 A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
What Do Podiatrists Do?
Podiatrists are physicians, and often surgeons, who have studied the foot, ankle, and lower leg, along with all associated ailments. They have received an undergraduate degree as well as medical degree and undergo four years of postgraduate study with a three-year residency. They treat a variety of foot and ankle issues, including fungal and ingrown toenails, heel pain, fractures, ankle sprains and strains, nerve damage (neuromas), bunions, hammertoe, arthritis, wound care, and complications of the feet due to diabetes and peripheral artery disease, and much more. They can also perform surgeries to treat certain foot and ankle conditions, perform gait analyses, and fit and create custom orthotics for their patients. If you experience any discomfort in your feet or ankles or are having a hard time getting around, make an appointment with a podiatrist who can get to the bottom of your condition and treat it accordingly.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot care needs.